what is the term for the puncture of the chest wall to remove fluid?
| Thoracentesis | |
|---|---|
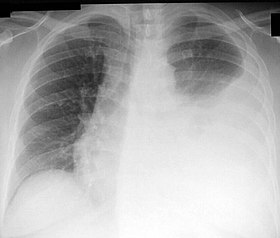 Breast X-ray showing a left-sided pleural effusion (right side of image). This can be treated with thoracentesis. | |
| ICD-9-CM | 34.91 |
| Other codes | OPCS-4.twoT12.3 |
| MedlinePlus | 003420 |
Thoracentesis , also known as thoracocentesis (from Greek θώραξ thōrax 'chest, thorax'—GEN thōrakos—and κέντησις kentēsis 'pricking, puncture'), pleural tap, needle thoracostomy, or needle decompression (often used term) is an invasive medical procedure to remove fluid or air from the pleural infinite for diagnostic or therapeutic purposes. A cannula, or hollow needle, is carefully introduced into the thorax, mostly later on administration of local anesthesia. The procedure was first performed by Morrill Wyman in 1850 and so described by Henry Ingersoll Bowditch in 1852.[one]
The recommended location varies depending upon the source. Some sources recommend the midaxillary line, in the eighth, ninth, or tenth intercostal space.[two] Whenever possible, the procedure should be performed under ultrasound guidance, which has shown to reduce complications.[three] [iv] [v]
Tension pneumothorax is a medical emergency that requires emergent needle decompression before a chest tube is placed.[6] [7]
Indications [edit]

The analogy shows a person having thoracentesis. The person sits upright and leans on a tabular array. Excess fluid from the pleural space is tuckered into a bag.

Instruments for thoracocentesis and needle biopsy of the pleura.[8]
This procedure is indicated when unexplained fluid accumulates in the chest cavity exterior the lung. In more than xc% of cases analysis of pleural fluid yields clinically useful information. If a big corporeality of fluid is present, and then this procedure can also be used therapeutically to remove that fluid and improve patient comfort and lung office.
The virtually common causes of pleural effusions are cancer, congestive heart failure, pneumonia, and recent surgery. In countries where tuberculosis is mutual, this is also a common cause of pleural effusions.
When cardiopulmonary status is compromised (i.e. when the fluid or air has its repercussions on the part of eye and lungs), due to air (significant pneumothorax), fluid (pleural fluid) or blood (hemothorax) outside the lung, then this procedure is usually replaced with tube thoracostomy, the placement of a large tube in the pleural space.
Contraindications [edit]
An uncooperative patient or a coagulation disorder that cannot exist corrected are relative contraindications.[nine] Routine measurement of coagulation profiles is mostly non indicated, however; when performed past an experienced operator "hemorrhagic complications are infrequent after ultrasound-guided thoracentesis, and attempting to correct an aberrant INR or platelet level before the procedure is unlikely to confer any benefit."[x]
Relative contraindications include cases in which the site of insertion has known bullous emphysema, use of positive finish-expiratory force per unit area (PEEP, come across mechanical ventilation) and only one operation lung (due to diminished reserve). Traditional expert opinion suggests that the aspiration should not exceed 1L to avoid the possible development of pulmonary edema, but this recommendation is uncertain every bit the volume removed does non correlate well with this complexity.[five]
Complications [edit]
Major complications are pneumothorax (iii–30%), hemopneumothorax, hemorrhage, hypotension (low blood pressure due to a vasovagal response) and reexpansion pulmonary edema.
Pocket-size complications include a dry tap (no fluid render), subcutaneous hematoma or seroma, feet, dyspnea and cough (afterward removing large book of fluid).
The utilize of ultrasound for needle guidance can minimize the complication rate.[three] [4] [5]
Follow-upward imaging [edit]
While chest X-ray has traditionally been performed to assess for pneumothorax following the process, information technology may no longer be necessary to exercise then in asymptomatic, non-ventilated persons given the widespread use of ultrasound to guide this procedure.[11]
Interpretation of pleural fluid assay [edit]
Several diagnostic tools are available to determine the etiology of pleural fluid.
Transudate versus exudate [edit]
First the fluid is either transudate or exudate.
An exudate is divers as pleural fluid to serum full poly peptide ratio of more than 0.5, pleural fluid to serum LDH ratio > 0.six, and accented pleural fluid LDH > 200 IU or > 2/3 of the normal.
An exudate is defined as pleural fluid that filters from the circulatory system into lesions or areas of inflammation. Its composition varies but generally includes water and the dissolved solutes of the main circulatory fluid such as claret. In the case of claret it will contain some or all plasma proteins, white claret cells, platelets and (in the instance of local vascular impairment) crimson claret cells.
Exudate
- hemorrhage
- Infection
- Inflammation
- Malignancy
- Iatrogenic
- Connective tissue illness
- Endocrine disorders
- Lymphatic disorders vs Constrictive pericarditis
Transudate
- Congestive heart failure
- Nephrotic syndrome
- Hypoalbuminemia
- Cirrhosis
- Atelectasis
- trapped lung
- Peritoneal dialysis
- Superior vena cava obstruction
Amylase [edit]
A high amylase level (twice the serum level or the absolute value is greater than 160 Somogy units) in the pleural fluid is indicative of either acute or chronic pancreatitis, pancreatic pseudocyst that has dissected or ruptured into the pleural space, cancer or esophageal rupture.
Glucose [edit]
This is considered low if pleural fluid value is less than l% of normal serum value. The differential diagnosis for this is:
- rheumatoid effusion. The levels are characteristically depression (<fifteen mg/dL).
- lupus effusion
- bacterial empyema
- malignancy
- tuberculosis
- esophageal rupture (Boerhaave syndrome)
pH [edit]
Normal pleural fluid pH is approximately 7.threescore. A pleural fluid pH below 7.30 with normal arterial claret pH has the aforementioned differential diagnosis every bit low pleural fluid glucose.
Triglyceride and cholesterol [edit]
Chylothorax (fluid from lymph vessels leaking into the pleural crenel) may be identified by determining triglyceride and cholesterol levels, which are relatively high in lymph. A triglyceride level over 110 mg/dl and the presence of chylomicrons indicate a chylous effusion. The appearance is generally milky but can be serous.
The main crusade for chylothorax is rupture of the thoracic duct, most frequently as a result of trauma or malignancy (such as lymphoma).
Cell count and differential [edit]
The number of white blood cells tin can requite an indication of infection. The specific subtypes tin also give clues equally to the blazon on infection. The amount of cherry-red blood cells are an obvious sign of bleeding.
Cultures and stains [edit]
If the effusion is acquired past infection, microbiological culture may yield the infectious organism responsible for the infection, sometimes before other cultures (e.m. claret cultures and sputum cultures) become positive. A Gram stain may requite a rough indication of the causative organism. A Ziehl–Neelsen stain may place tuberculosis or other mycobacterial diseases.
Cytology [edit]
Cytology is an important tool in identifying effusions due to malignancy. The most common causes for pleural fluid are lung cancer, metastasis from elsewhere and pleural mesothelioma. The latter often presents with an effusion. Normal cytology results do not reliably dominion out malignancy, but make the diagnosis more unlikely.
References [edit]
- ^ Kelly, Howard A.; Burrage, Walter L. (eds.). . . Baltimore: The Norman, Remington Visitor.
- ^ "Human being Gross Anatomy". Archived from the original on 2008-02-14. Retrieved 2007-10-22 .
- ^ a b Gordon, Craig Eastward.; Feller-Kopman, D; Cramp, EM; Smetana, GW (22 February 2010). "Pneumothorax Post-obit Thoracentesis". Athenaeum of Internal Medicine. 170 (four): 332–9. doi:10.1001/archinternmed.2009.548. PMID 20177035.
- ^ a b Feller-Kopman, David (July 2007). "Therapeutic thoracentesis: the role of ultrasound and pleural manometry". Current Opinion in Pulmonary Medicine. 13 (4): 312–318. doi:ten.1097/MCP.0b013e3281214492. PMID 17534178.
- ^ a b c Daniels, Craig Due east; Ryu, Jay H (July 2011). "Improving the safety of thoracentesis". Current Stance in Pulmonary Medicine. 17 (iv): 232–236. doi:10.1097/MCP.0b013e328345160b. PMID 21346571.
- ^ Harcke, HT; Mabry, RL; Mazuchowski, EL (2013). "Needle thoracentesis decompression: observations from postmortem computed tomography and autopsy". Periodical of Special Operations Medicine. 13 (4): 53–eight. PMID 24227562.
- ^ Ball, Chad 1000.; Wyrzykowski, Amy D.; Kirkpatrick, Andrew W.; Dente, Christopher J.; Nicholas, Jeffrey Chiliad.; Salomone, Jeffrey P.; Rozycki, Grace South.; Kortbeek, John B.; Feliciano, David Five. (2010). "Thoracic needle decompression for tension pneumothorax: clinical correlation with catheter length". Canadian Journal of Surgery. 53 (3): 184–188. PMC2878990. PMID 20507791.
- ^ de Menezes Lyra R (1997). "A modified outer cannula can help thoracentesis subsequently pleural biopsy". Breast. 112 (1): 296. doi:10.1378/chest.112.1.296. PMID 9228404.
- ^ "Thoracentesis (department)". Merck Manual. Merck Manual. Retrieved seven November 2014.
- ^ Hibbert, Rebecca One thousand.; Atwell, Thomas D.; Lekah, Alexander; Patel, Maitray D.; Carter, Rickey E.; McDonald, Jennifer Southward.; Rabatin, Jeffrey T. (Baronial 2013). "Safety of Ultrasound-Guided Thoracentesis in Patients With Abnormal Preprocedural Coagulation Parameters". Chest. 144 (2): 456–463. doi:10.1378/breast.12-2374. PMID 23493971.
- ^ Petersen, William Grand.; Zimmerman, Robert (Apr 2000). "Limited Utility of Breast Radiograph After Thoracentesis". Chest. 117 (4): 1038–1042. doi:10.1378/chest.117.4.1038. PMID 10767236.
External links [edit]
-
 Media related to Thoracentesis at Wikimedia Eatables
Media related to Thoracentesis at Wikimedia Eatables - A photograph gallery of thoracentesis showing the procedure step-by-step. V. Dimov, B. Altaqi, Clinical Notes, 2005. A gratuitous PDA version.
Source: https://en.wikipedia.org/wiki/Thoracentesis
0 Response to "what is the term for the puncture of the chest wall to remove fluid?"
Post a Comment